Miscarriage
TREATMENT OF MISCARRIAGE
Are you frequently experiencing Miscarriages?

Or are you fearful of bearing one? Please Consult Our Best Gynecologist in Lahore Pakistan,
If you are experiencing any miscarriage symptoms like:
If you experience any of these symptoms, contact our gynecologist immediately. We have top-notch treatments for you.
TREATMENT OF MISCARRIAGE
Need to know about Miscarriage
A miscarriage (abortion) is the unexpected termination of a pregnancy within the first 20 weeks of pregnancy. Most miscarriages are out of your control and happen because the fetus stops developing.
A miscarriage is a spontaneous loss before the 20th week; roughly 10% to 20% of pregnancies end in miscarriage. But the actual number is likely higher because many miscarriages occur early in pregnancy before you know you're pregnant.
The term "miscarriage" may indicate a problem during pregnancy. But this is rarely true. Most miscarriages emerge because the fetus does not grow as expected.
Abortion is an emotional experience that doesn't make it any easier. Chromosomal problems cause most miscarriages.
Common Types of Miscarriages In Pakistan Women Faces
These are a few types of miscarriages you can experience:
▪ Missed miscarriage: There are no miscarriage symptoms, but the ultrasound confirms that the fetus is not beating.
▪ Complete miscarriage: In the case of a complete miscarriage, the uterus is empty—profuse bleeding and expulsion of fetal tissue. Our doctors can confirm a complete miscarriage with an ultrasound.
▪ Recurrent Miscarriage: Three consecutive spontaneous miscarriages. It affects about 1% of couples.
▪ Threatened miscarriage: Your cervix remains closed, but you bleed and have pelvic cramps. Pregnancy usually has no further problems. Our doctors will closely monitor the remainder of the pregnancy.
▪ Inevitable miscarriage: Heavy bleeding, cramping, and the cervix has started to open (dilate). You can leak amniotic fluid. There is a high chance of a complete miscarriage.
Symptoms of a miscarriage
Signs and symptoms of miscarriage may include:
- Vaginal spotting or bleeding
- Abdominal or lower back pain or cramping
- Fluid or tissue from the vagina
If you pass fetal tissue from your vagina, put it in a clean container and take it to a doctor or hospital for testing.
Most women who experience vaginal spotting or bleeding during the first trimester can have a successful pregnancy.
Causes of miscarriage
Chromosomal abnormalities cause most miscarriages in the first trimester (up to 13 weeks). They (chromosomes) are tiny structures within human cells that carry genes.
Most chromosomal problems occur by chance. Several factors that can lead to miscarriage are:
Stress, exercise, sexual activity, or long-term use of birth control pills can cause miscarriage. Regardless of your situation, it's important not to blame yourself for a miscarriage. Most miscarriages have nothing to do with what you did or didn't do.
TREATMENT OF MISCARRIAGE
Genetic or chromosomal problems
Above all, the reason for most miscarriages is that the fetus does not mature as predicted. About 50% of miscarriages are associated with extra or missing chromosomes. Most of the time, chromosomal problems result from an accidental error that occurs when the embryo divides and grows rather than a problem inherited from the parents.
Chromosomal problems can cause:
TREATMENT OF MISCARRIAGE
The risk factor in Miscarriage
Risk factors are the things that increase the likelihood of miscarriage.
TREATMENT OF MISCARRIAGE
Complications in Miscarriage
Some women who have miscarried develop uterine infections. This is also called a septic abortion. However, some common complication signs include:
Prevention To Avoid Miscarriage
Here are a few things that you should do to prevent a miscarriage. To avoid, protect yourself from any mishap;
Diagnosis and Testing for Miscarriage
Our doctor will perform an ultrasound to confirm the miscarriage. These tests check for the fetus's heartbeat or the presence of a yolk sac (one of the first fetal structures a doctor can see on an ultrasound).
You need a blood test (HCG) to measure a hormone produced by the placenta. A low HCG level confirms a miscarriage.
TREATMENT OF MISCARRIAGE
Treatment for Miscarriages
There are two types of treatment;
- Non-Surgical treatment
- Surgical treatment
Non-surgical treatment for miscarriage
Our doctor may recommend waiting if the pregnancy goes away on its own. This may be the case if you have missed a miscarriage. It can take a few days for a miscarriage to begin. If it is not safe to wait for the tissue to pass, or if you wish to have the tissue removed as soon as possible, you may be advised to take medication to help the uterus to expel the pregnancy. These options are usually only available if you have a miscarriage in the first ten weeks of pregnancy.
If a miscarriage is not confirmed, but you have symptoms of a miscarriage, our doctor may order a few days of bed rest. You may be admitted to the hospital overnight for monitoring. When the bleeding stops, you may be able to continue your normal activities. If the cervix is dilated, you may be diagnosed with cervical insufficiency and have surgery to close the cervix (cerclage).
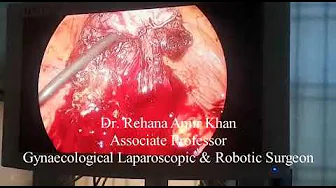
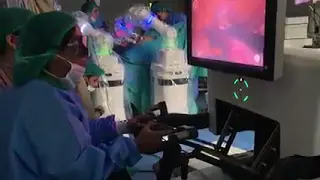
Surgical treatment for miscarriages
If your uterus is not experiencing pregnancy or heavy bleeding, our doctor may advise suction evacuation rather than D&C. Surgery may also be the only option if you are after ten weeks of pregnancy. During these procedures, the cervix is dilated, and any remaining pregnancy-related tissue is scraped or gently aspirated out of the uterus. Our doctors perform these procedures in the hospital, and you will be sedated.
What tests should be done after repeated miscarriage?
You may need blood tests or genetic testing if you have had more than three consecutive miscarriages (called recurrent miscarriages). These include:
Our gynecologist in Lahore may also examine your uterus using one of the following methods: